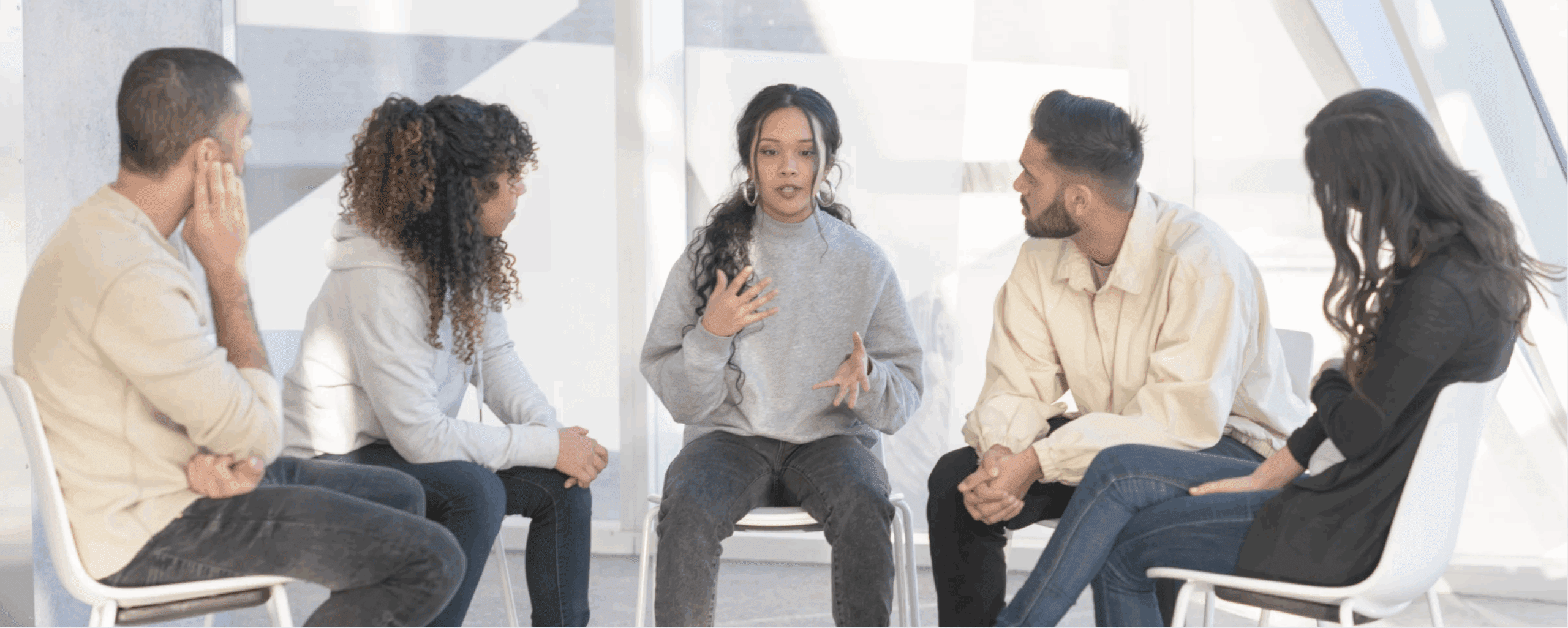
Whether you struggle with depression yourself or have watched someone you love battle with the condition, you’ve probably seen the impacts of depression.
While society has made strides in mental health awareness, the world still has a long way to go in dismantling the stigma attached to depression. The topic of depression is weighed down with misinformation and minimization, which can understandably make people struggling with the condition feel defeated and hopeless.
To combat the stigma around mental health, you can learn more about depressive disorders. If you or someone you love struggles with depression, here are 10 facts about depression that can give you a better understanding of depression’s impact.
What Is Depression?
When most people think of depression, they may picture the symptoms of major depressive disorder (MDD). If you suffer from major depressive disorder, also known as clinical depression, you experience the most severe form of this mental health disorder.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the definition of a major depressive episode (MDE) is “a period of at least two weeks when a person experienced a depressed mood or loss of interest or pleasure in daily activities, and had a majority of specified symptoms, such as problems with sleep, eating, energy, concentration, or self-worth.”
In general, people with depression can’t experience the joys of life, and things that once made them happy become a bitter reminder of what they no longer feel—happiness.
Feelings of sadness and apathy make daily tasks near impossible to accomplish. If you have an MDD, you might feel debilitating guilt and shame from canceling plans and self-isolating from loved ones. Paradoxically, you may sleep all day and wake up exhausted, or lay awake all night ruminating over past embarrassments or future failures.
Signs of depression can differ from person to person, but there are some common warning signs to look out for in yourself or a loved one.
Common signs of depression include:
- Persistent sad, “empty,” or anxious mood
- Loss of interest or pleasure in activities that were once enjoyed
- Decreased energy, fatigue, and increased need for sleep
- Difficulty concentrating, remembering, or making decisions
- Feelings of worthlessness, hopelessness, or guilt
- Thoughts of death or suicide
If you or someone you know is experiencing these symptoms, it’s important to seek professional help. Depression is a treatable condition but left untreated, it can lead to serious consequences. If you think you may be depressed, please contact your doctor for an evaluation.
1. Depression Isn’t Sadness
Depression is more than simply feeling bummed out for a few days. While feelings of sadness typically occur after an upsetting event, people with depression struggle to feel excitement, happiness, or motivation regardless of the situation.
While depression can affect everyone differently, the disorder often negatively impacts your emotions, behaviors, and thoughts.
Emotional signs of depression include:
- Sadness
- Anger
- Guilt
- Hopelessness
Behavioral changes during depression include:
- Social withdrawal
- A lack of energy
- Poor concentration
- Sleep problems
- Appetite changes
Thoughts caused by depressive disorders include:
- Low self-esteem
- Loss of interest in regular activities
- Thoughts of death or suicide
From time to time, hurtful situations can make you feel unmotivated and avoidant. Taking time to wallow or distract yourself from the pain you feel will often give you time to heal. Depression, however, is an illness that extends your sadness far past a typical mourning period. While feeling sad is a part of life, depression doesn’t have to be.
If you recognize these symptoms in yourself or a loved one, seek help from a mental health professional. It is important to share your experience with someone you trust because depression is a severe mental health disorder that can be debilitating if left untreated.
2. Depression Disrupts Your Brain Functions
Depressive disorders can affect neurotransmitters inside the brain, harming your ability to function properly. This is because many neurotransmitters play important roles in regulating your mood.
Known neurotransmitters affected by depression include:
- Serotonin
- Norepinephrine
- Dopamine
If you suffer from depression, your brain is likely unable to produce the appropriate amounts of neurotransmitters. When the brain can’t produce or absorb enough of certain chemicals, you end up feeling depressed.
For example, serotonin is one of the most commonly associated brain chemicals affected by depression. Known as the “feel-good” chemical, serotonin helps the brain regulate your mood and benefits your sense of well-being. When you are in a deep depression, the symptoms of fatigue and hopelessness are partially due to the lack of serotonin in your brain.
Similarly, dopamine—AKA the “pleasure” chemical—helps your brain in regulating emotion, memory, and thinking. More importantly, high dopamine levels produce the sensation of motivation and reward. Typically, people with mood disorders have low dopamine levels. As a result, you don’t feel motivated or accomplished.
As one of the main chemicals released during your body’s “fight or flight response,” norepinephrine increases your heart rate and blood pressure during moments of stress. If you, like many other people with depression, experience chronic symptoms of stress, your brain is constantly releasing norepinephrine. As a result, depressed people eventually struggle with low norepinephrine levels and lack the energy to take action and concentrate.
3. There Are 8 Depressive Disorder Types
Many believe that all depressed individuals have the same general experience. Similarly, some think that all depressive symptoms are a result of clinical depression.
However, depression comes in a variety of forms, making the term nuanced and distinct from one depressive disorder to the next. In fact, there are eight different types of depression, each with its own set of symptoms.
The eight types of depressive disorders include:
- Major depressive disorder (MDD)
- Persistent depressive disorder (PDD)
- Manic depression (bipolar disorder)
- Seasonal affective disorder (SAD)
- Psychotic depression
- Peripartum (postpartum) depression (PPD)
- Premenstrual dysphoric disorder
- Atypical depression
You may also experience situational depression, which happens in response to a stressful event. However, it is considered an adjustment disorder because it is a direct reaction to a painful situation that typically lessens in severity after several months.
That being said, the four most common types of depressive disorders are:
- Major depressive disorder (MDD)
- Persistent depressive disorder (PDD)
- Bipolar disorder (BD)
- Seasonal affective disorder (SAD)
4. Women Are More Likely to Be Depressed Than Men
In general, women have a higher risk of developing clinical depression. In fact, a study examining the gender differences in depression found that roughly twice as many women as men experience depressive symptoms.
A CDC study shows that about 1 in 10 women in the United States experienced a major depressive episode in the last year. Several factors may increase a woman’s risk of depression.
Risk factors found in women include:
- Puberty and hormonal fluctuations
- Premenstrual dysphoric disorder (PMDD)
- Unequal power dynamics
- Work overload
- Societal expectations
- Sexual or physical abuse
- Pregnancy hormones and complications
- Perinatal depression
- Postpartum depression (PPD)
- Perimenopause and menopause
Women are at a greater risk of developing depression due to the near-constant hormonal changes that occur within female reproductive organs. As a result, women are more likely to experience immense amounts of emotional distress. It can be difficult to talk about for many women due to the stigma surrounding menstrual cycles.
Some mood changes and depressed feelings occur with normal hormonal changes. While hormonal changes don’t cause depression by themselves, other biological, genetic, and personal circumstances put women at a higher risk of developing a depressive disorder.
5. Depression Is Linked to Genetics, Environment, and Mindset
Depression is thought to be caused by a combination of genetic, biological, environmental, and psychological factors.
The main influencing factors for depression include:
- Brain chemistry
- Genetics
- Personality
- Environment
Depression can be hereditary, meaning your genes play a role. If you have a depressed parent or a sibling, research shows that you are 2 or 3 times more likely to develop depression compared to the average person.
Similarly, depression has been shown to affect your brain chemistry. Specifically, depressive disorders disrupt the absorption of chemicals such as serotonin, norepinephrine, and dopamine.
Understandably, depression is more common in people who have low self-esteem or are generally pessimistic. For example, someone who is always seeing the worst in every situation and putting themselves down for past failures is far more likely to develop depression than the average person.
As with most mental health disorders, your environment can always make an impact on the development and severity of depressive symptoms. For instance, if you have lived through abuse, violence, poverty, or neglect, you are more likely to develop a depressive disorder.
6. Depression Affects More Than Your Mood
Most people have a general idea about the emotional impact of depression, but many people don’t know about the physical ramifications. In fact, depressed people can struggle with chronic pain or other distressing symptoms.
As a result, the physical effects of depression aren’t all in your head. In fact, research shows that depressed people often experience physical symptoms. So much so, vague feelings of soreness and pain are common reasons people seek help for depression.
Physical symptoms of depression include:
- Joint, limb, and back pain
- Stomach pain
- Fatigue
- Difficulty sleeping
- Appetite changes
- Weight gain/loss
- Psychomotor changes (decreased hand-eye coordination and reaction time)
- Vertigo/dizziness
- Overheating
- Hallucinations
Studies have also found that several different physical conditions are commonly associated with depression. Similarly, people with physical illnesses are at a significantly higher risk of developing a depressive disorder, which can worsen the symptoms of their physical condition.
For example, chronic pain can trigger a depressive episode because nonstop pain makes you vulnerable to feelings of hopelessness and despair. On the flip side, depressed people can develop chronic pain as a result of their brain mixing up signals that cause physical distress.
Diseases linked to depression include:
- Heart disease
- Stroke
- Diabetes
- Arthritis
- Kidney disease
- HIV and AIDS
- Lupus
- Multiple sclerosis (MS)
- Chronic fatigue syndrome (CFS)
- Fibromyalgia (FM)
- Irritable bowel syndrome (IBS)
- Multiple chemical sensitivity (MCS)
- Myocardial infarct (MI)
A study found that severe depression is associated with a significant decrease in heart rate variability in patients with stable coronary heart disease (recurring episodes). As a result, depressed people, who are more likely to develop chronic physical conditions like heart disease, are at a higher risk of experiencing worse symptoms following a heart attack due to higher levels of stress on their heart.
7. Depression Can Lead to Substance Abuse
Research shows that mood disorders such as depression and bipolar disorder are the most common co-occurring disorders found in people with substance use disorders (SUD).
Depression changes the way you feel, think, and behave. Oftentimes, the physical and emotional distress can make people desperate for relief. As a result, you may begin to misuse substances in order to ease the symptoms of your disorder.
According to the National Institute of Mental Health (NIMH), roughly 50% of individuals with SUD have a co-occurring mental health disorder, like depression. While feelings of hopelessness can lead to substance abuse, SUDs can also cause depression. Like depression, substance use disorders can trigger changes in the brain that increase the risk of developing a mental health disorder.
Both depression and SUDs affect people from around the world. Co-occurring substance use disorders and depressive disorders are also both common and can result in an untimely death, especially when they overlap. If you are struggling with depression and substance abuse, it is important to know that your symptoms are treatable and you can recover.
8. Depression Is a Worldwide Disorder
Depression is a common mental disorder, affecting approximately 5% of all adults. Around the world, depression affects about 1 in 15 adults each year. Also, 1 in 6 people will experience symptoms of a depressive disorder at some time in their life.
In 2021, the World Health Organization (WHO) estimated roughly 3.8% of the world’s population has depression—280 million people worldwide.
Due to depression’s impact on a person’s productivity, the disorder can cause issues at work, school, home, and everything in between. This can lead to extreme distress and even end in suicide. Across the globe, more than 700,000 people die from suicide each year. In fact, suicide is the 4th leading cause of death for people ages 15 to 29.
9. America Is Depressed
The 2020 National Survey on Drug Use and Health (NSDUH) found that 8.4% of all U.S. adults, or an estimated 21 million adults, had at least one major depressive episode. The survey also shows that 6% of all U.S. adults, just shy of 15 million, had at least one major depressive episode with severe impairment in the past year.
In the U.S., the adult populations experiencing the highest rates of major depressive episodes include:
- Females
- Multi-racial people
- Adults between the ages of 18-25
According to the Pan American Health Organization (PAHO), by the time Americans reach the age of 20, 41% will develop common mental health disorders, including depression, self-harm, and anxiety.
10. Depression Is Treatable
Even though depression is one of the most common mental disorders in the United States, everyone experiences it differently.
As a result, there is no “one-size-fits-all” for treatment. In fact, it’s common to try multiple treatment methods before finding the right one for you. While treatment may take time, finding the treatment will make a world of a difference.
That being said, there are several effective treatments available to help manage your symptoms. If traditional treatments have been unsuccessful, there are alternative and experiential therapies that you might find more impactful. There are also new FDA-approved treatment approaches available.
In order to benefit from behavioral health and medical care, the treatment approaches should be tailored to best suit your symptoms and overall wellness. A common approach in the treatment of depression is a combination of therapy, medication, and lifestyle changes.
How Do I Know If I Have Depression?
If you’re concerned that you may be suffering from depression, getting evaluated by a licensed physician or behavioral health care provider is the best next step to take. If you share that you’re suffering from nonstop sadness or neverending apathy, your healthcare provider may perform a mental health assessment that is more or less a depression test. These evaluations usually include a series of questions on a scale of 1 to 5.
In general, tests for depression outline the signs and symptoms of the disorder. Your answers will determine the:
- Type of depression
- Level of severity
- Existence of any co-occurring disorders
- Best course of action in building your treatment plan
Reach Out for Support
If you or a loved one needs help, please feel free to reach out to us at 877-RECOVERY. Our addiction specialists are available 24/7 to assist you through this time and help you find hope in recovery.
Call or Text 988
Substance Abuse and Mental Health Services Administration (SAMHSA) Helpline
Call 1-800-622-4357 or Text 435748 (HELP4U)
Text HOME to 741741